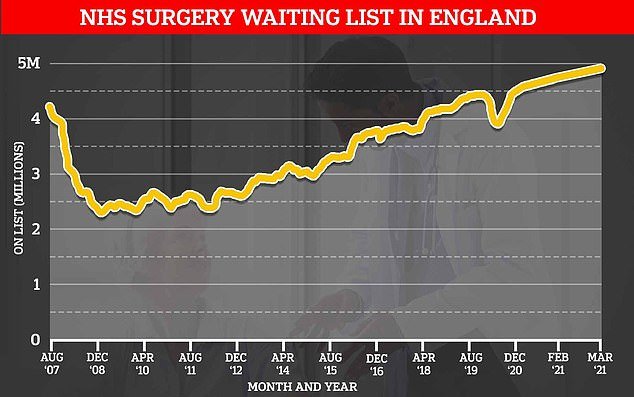
Nearly 5million people in England are waiting for hospital treatment — the highest number ever recorded.
Despite the second Covid wave having been almost entirely squashed, the NHS is still struggling to recover from the impact of the virus on normal care.
Some 4.95million people were waiting to start routine treatment in March, the most since records began in 2007, according to NHS England statistics published today.
They also showed that the number waiting more than a year to get hospital care in March stood at 436,127. This is the highest number in a single calendar month since August 2007, when the figure was 578,682.
The Royal College of Surgeons branded the numbers ‘stomach-churning’, saying Britons living with pains and illnesses had been ‘forced to put their lives on hold’ due to the pandemic.
Pre-lockdown figures show just 3,000 patients were waiting more than a year to start hospital treatment in March 2020.
The NHS figures look at patients waiting for routine surgeries such as hip and knee operations, cochlear implants and vascular operations. These procedures have repeatedly been delayed during the crisis as the NHS turned its attention to dealing with influxes of Covid patients.
It comes as health leaders called for social distancing rules in hospitals to be loosened so doctors can get through the backlog quicker.
NHS bosses last night announced another £160million in funding to help tackle the waiting list, with virtual wards, 3D eye scanners and at-home antibiotic kits among new initiatives to be trialled.
NHS England statistics show more patients are on the waiting list since the previous record in August 2007, when health leaders first started collecting the figures
The number of people on waiting lists for routine surgery in England has risen by 250,000, or five per cent, since February, despite routine surgery restarting when the second Covid wave died down.
Tim Mitchell, the vice-president of the Royal College of Surgeons of England, suggested officials had become desensitised to the knock-on effects of shutting down NHS services to tackle the pandemic.
He said: ‘In recent months we’ve become accustomed to seeing the record broken each month for the number of people waiting for NHS hospital treatment.
‘But we must not forget that behind these stomach-churning numbers are ordinary people who have been forced to put their lives on hold. Today’s figures show the impact that a year of Covid has had on NHS surgery.’
In a letter to the health secretary, Matt Hancock, health leaders asked for strict social distancing rules to be eased in hospitals so the NHS can seize on a ‘summer of opportunity’ and get through as many patients as possible.
The NHS Confederation said the success of the vaccine rollout means people can safely be seen in clinics.
At the moment, Covid rules mean hospitals can only operate at about 60 per cent capacity.
Danny Mortimer, interim chief executive of the confederation, told The Times that clinics wanted to ‘just see if they could get an extra 10 or 15 per cent, in terms of patient numbers that they could see’.
He suggested six-bed bays in hospitals that contained only three patients could be extended to four or five, for example.
NHS England figures also showed A&E emergency attendances in April were more than double the levels the previous month, after 1.87million were registered.
But this was likely a reflection of lower-than-usual numbers the same time the previous year because it was during the first lockdown.
NHS England said the health service had seen almost a quarter of a million people with suspected cancer in March as services ‘began to bounce back’ after the peak of the winter Covid wave.
Dame Cally Palmer, NHS cancer director, said: ‘From Covid-friendly cancer drugs to fast tracking specialist radiotherapy for patients, NHS staff have gone to great lengths to ensure cancer treatment could continue safely throughout the pandemic.
‘It is welcome news that more people than ever before came forward for potentially life-saving checks in March, with the vast majority being seen very quickly.’
Last night it was revealed the NHS is ploughing £160million into a series of trials to reduce waiting lists caused by the pandemic.
With cases now at their lowest levels since last summer, health officials hope to start making inroads into the millions of people needing routine surgery and care.
NHS England has earmarked between £10-20 million each to 15 pilot schemes across the country.
These include a cataract clinic designed to perform hundreds of procedures a day in Devon, surgical hubs in London and mobile cancer screening units in Nottingham.
Over the next three months, tens of thousands of patients across the country will be asked to trial the new facilities such as one-stop testing facilities and pop-up clinics.
Virtual wards and home assessments, 3D eye scanners, at-home antibiotic kits, ‘pre-hab’ for patients about to undergo surgery, AI in GP surgeries and ‘Super Saturday’ clinics, where multi-disciplinary teams come together at the weekend to offer more specialist appointments, will also be trialled.
Officials hope these ‘new ways of doing things’ will increase the numbers of tests and treatments as they did before the pandemic, while helping to develop a blueprint to implement on a nationwide scale.